Testosterone, often misunderstood as merely a “sex hormone,” is actually a fundamental component of male health affecting everything from cognitive function to cardiovascular health. Yet millions of men experience declining testosterone levels without recognizing the cause of their symptoms.
This comprehensive guide cuts through the marketing hype and misinformation to deliver evidence-based insights on recognizing low testosterone symptoms and implementing effective strategies to reverse them. Whether you’re in your 30s noticing the first signs of hormonal change or in your 60s seeking to regain vitality, understanding the truth about testosterone is the first step toward optimization.
Understanding Testosterone’s Widespread Impact
The Fundamental Role of Testosterone
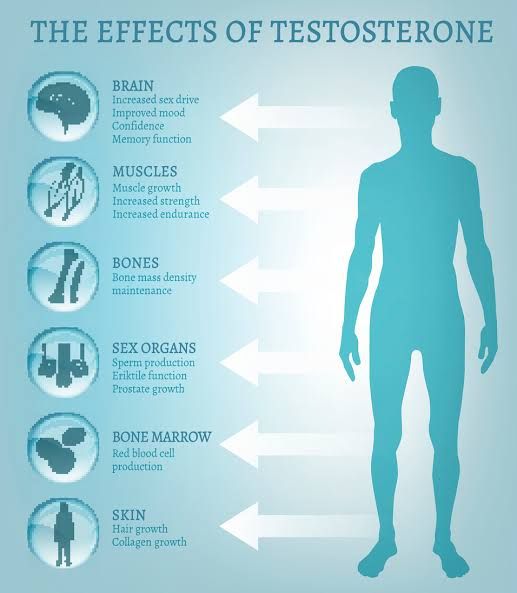
Testosterone is far more than just a driver of sexual function and muscle development. This crucial hormone influences nearly every system in the male body:
- Brain function: Supports cognitive clarity, motivation, and mood stability
- Cardiovascular system: Promotes healthy blood vessel function and heart health
- Metabolism: Regulates insulin sensitivity, fat distribution, and energy production
- Musculoskeletal system: Maintains muscle mass, bone density, and joint health
- Immune system: Modulates immune responses and inflammation
- Sleep regulation: Influences sleep architecture and quality
When testosterone levels decline, the effects ripple throughout these systems, often creating a cascade of seemingly unrelated symptoms that many men and even some healthcare providers fail to connect.
The Normal vs. Optimal Debate
One of the most confusing aspects of testosterone health involves laboratory reference ranges. Most labs consider “normal” total testosterone to fall between 250-1000 ng/dL—an extremely wide range reflecting population averages rather than optimal health.
Research increasingly suggests that symptoms often appear when levels fall below 550 ng/dL, despite remaining technically within “normal” range. This creates a problematic gap where men experience clear symptoms but are told their levels are “normal.”
Dr. Thomas O’Connor, a leading physician specializing in hormonal health, explains: “The problem isn’t just low testosterone—it’s suboptimal testosterone. A man at 320 ng/dL is technically ‘normal’ according to many labs, but he’s likely experiencing significant symptoms that impact quality of life.”
Recognizing the Symptoms – Beyond Sex Drive
The symptoms of low testosterone can be insidious, often attributed to aging, stress, or lifestyle factors. Recognizing the constellation of symptoms is crucial for proper identification.
Physical Symptoms
- Body composition changes: Increased abdominal fat despite diet consistency; difficulty gaining or maintaining muscle mass even with regular training
- Fatigue and energy disruption: Persistent tiredness unrelieved by rest; afternoon energy crashes; decreased exercise recovery capacity
- Sleep disturbances: Difficulty falling or staying asleep; unrefreshing sleep despite adequate duration
- Physical performance decline: Reduced strength, endurance, and athletic output not explained by training changes
- Cardiovascular changes: Decreased exercise tolerance; mild blood pressure elevations; unfavorable lipid profile shifts
Cognitive and Emotional Symptoms
- Mental fog: Reduced cognitive sharpness; difficulty concentrating; memory lapses
- Motivation decrease: Procrastination in previously enjoyed activities; reduced drive at work or in personal projects
- Mood alterations: Increased irritability; emotional flatness; decreased stress resilience
- Confidence reduction: Diminished assertiveness; increased social anxiety; reduced leadership initiative
- Depression-like symptoms: Low mood states not meeting clinical depression criteria but impacting quality of life
Sexual Symptoms
- Libido changes: Decreased spontaneous sexual thoughts; reduced response to normal stimuli
- Erectile changes: Less firm erections; difficulty maintaining erections; reduced morning erections
- Sexual performance anxiety: New concerns about performance that create a negative feedback loop
- Delayed ejaculation: Increased time to orgasm; sometimes decreased orgasm intensity
- Reduced genital sensation: Subtle decreases in penile sensitivity
The Symptom Timeline: How Low T Typically Progresses
Low testosterone rarely appears suddenly with all symptoms at once. Instead, it typically follows a progression that can span years:
- Early phase (often 30s-40s): Subtle energy changes, occasional erectile inconsistency, slight body composition shifts
- Intermediate phase: More persistent fatigue, noticeable libido reduction, increased body fat despite exercise, mood fluctuations
- Advanced phase: Significant muscle loss, consistent erectile dysfunction, profound energy disruption, potential depression, cognitive impacts
Understanding this progression helps men identify issues earlier, when they’re more responsive to lifestyle interventions.
The Truth About Testosterone Decline
Debunking the “Inevitable Aging” Myth
While some testosterone decline with age is natural, the dramatic drops many men experience are neither inevitable nor untreatable. Research comparing modern men to historical populations suggests our baseline testosterone levels are falling independent of age:
- A 2007 Journal of Clinical Endocrinology and Metabolism study found that men today have approximately 20% less testosterone than men of the same age just two decades earlier
- Analysis of health records shows consistently declining testosterone levels across all age groups compared to historical norms
These findings suggest environmental and lifestyle factors play significant roles beyond natural aging.
The Primary Drivers of Low Testosterone
Modern research has identified several key factors driving testosterone decline:
- Chronic Stress: Elevated cortisol from persistent stress directly suppresses testosterone production while increasing aromatase activity (which converts testosterone to estrogen)
- Environmental Exposures: Endocrine-disrupting chemicals found in plastics, pesticides, personal care products, and food packaging interfere with hormonal signaling
- Metabolic Dysfunction: Insulin resistance, obesity, and metabolic syndrome create bidirectional negative effects on testosterone production
- Sleep Disruption: Poor sleep quality and insufficient duration impair the nighttime testosterone production cycle
- Nutritional Factors: Vitamin D deficiency, zinc insufficiency, and excessive consumption of processed foods all negatively impact testosterone synthesis
- Chronic Inflammation: Systemic inflammation from poor diet, environmental exposures, and chronic stress impairs testicular function and hormone signaling
- Sedentary Behavior: Lack of movement, particularly resistance training, fails to stimulate natural testosterone production pathways
Dr. Michael Eisenberg, Director of Male Reproductive Medicine at Stanford, notes: “We’re seeing testosterone declines that cannot be explained by aging alone. The evidence points to a combination of lifestyle, environmental, and metabolic factors that are collectively driving this trend.”
Comprehensive Testing Beyond Basic Blood Work
The Limitations of Standard Testing
Many men who suspect low testosterone encounter frustrating experiences with standard medical testing:
- Basic panels often measure only total testosterone, missing crucial markers
- Single-point morning testing can miss daily fluctuations
- Outdated reference ranges may label suboptimal levels as “normal”
The Complete Testosterone Assessment
A comprehensive evaluation should include:
- Total Testosterone: The baseline measurement of circulating testosterone
- Free Testosterone: The biologically active form available to tissues (often low despite normal total levels)
- Sex Hormone Binding Globulin (SHBG): The protein that binds testosterone, potentially making it unavailable to tissues
- Estradiol (E2): Elevated levels can cause overlapping symptoms with low testosterone
- Dihydrotestosterone (DHT): A potent metabolite that mediates some testosterone effects
- Luteinizing Hormone (LH) and Follicle Stimulating Hormone (FSH): Indicates whether the issue originates in the testes or the brain
- Complete Thyroid Panel: Thyroid dysfunction often accompanies testosterone issues
- Metabolic Markers: Including fasting glucose, insulin, HbA1c to identify insulin resistance
- Cortisol Testing: Preferably diurnal (4-point) testing to assess stress hormone patterns
- Inflammatory Markers: hsCRP, IL-6, and TNF-alpha to evaluate systemic inflammation
When and How to Test
For optimal accuracy:
- Test in the early morning (7-9am) when levels are naturally highest
- Maintain consistent sleep patterns before testing
- Consider multiple tests over time rather than single evaluations
- Fast for 12 hours before comprehensive panels
- Avoid high-intensity exercise for 24 hours before testing
The Lifestyle Intervention Hierarchy
Research demonstrates that specific lifestyle interventions can significantly impact testosterone levels, often without medication. These interventions follow a hierarchy of effectiveness:
1. Sleep Optimization: The Foundation
Nothing undermines testosterone more consistently than poor sleep. Studies show that just one week of restricted sleep (5-6 hours) can reduce testosterone by 10-15%.
Implementation strategy:
- Establish consistent sleep/wake times (even on weekends)
- Create a sleep sanctuary: cool (65-68°F), completely dark, and quiet
- Implement a 30-minute wind-down routine without screens
- Consider tracking sleep with an Oura Ring or similar device
- Target 7-9 hours of quality sleep nightly
2. Resistance Training: The Stimulus
Heavy compound exercises have been shown to acutely increase testosterone production while creating long-term improvements in hormonal baseline.
Implementation strategy:
- Prioritize compound movements: squats, deadlifts, presses, rows
- Train with moderate to heavy weights (70-85% of 1RM)
- Focus on progressive overload (gradually increasing weight/volume)
- Include 3-4 strength sessions weekly
- Limit excessive cardio, which can suppress testosterone when overdone
3. Nutritional Optimization: The Building Blocks
Diet provides both the macronutrients and micronutrients necessary for testosterone production.
Implementation strategy:
- Maintain sufficient caloric intake (severe restriction lowers testosterone)
- Consume adequate dietary fat (30-35% of calories), particularly monounsaturated and saturated fats
- Ensure sufficient protein (1g per pound of lean body mass)
- Include micronutrient-dense foods high in zinc, magnesium, and vitamin D
- Limit alcohol consumption (beyond 2 drinks daily shows hormonal impact)
- Minimize ultra-processed foods and added sugars
Key testosterone-supporting foods:
- Egg yolks (cholesterol is a precursor to testosterone)
- Oysters and shellfish (zinc)
- Grass-fed beef (zinc, vitamin D, healthy fats)
- Brazil nuts (selenium)
- Pomegranates (potent antioxidants)
- Cruciferous vegetables (help manage estrogen)
4. Stress Management: The Protector
Chronic stress directly suppresses testosterone while increasing cortisol, creating a hormonal environment unconducive to optimization.
Implementation strategy:
- Implement daily deliberate stress reduction practices (meditation, breathing exercises)
- Create clear work/life boundaries
- Practice regular nature exposure (“forest bathing”)
- Consider heat exposure via sauna (shown to boost testosterone)
- Implement strategic cold exposure
5. Environmental Detoxification: The Defense
Reducing exposure to endocrine-disrupting chemicals can help remove obstacles to natural testosterone production.
Implementation strategy:
- Replace plastic food storage with glass or stainless steel
- Filter drinking water
- Choose organic produce when possible (especially for the “dirty dozen”)
- Use natural personal care products
- Avoid thermal receipt paper (high in BPA)
- Regularly clean indoor air with proper filtration
6. Strategic Supplementation: The Support
While supplements cannot overcome poor lifestyle fundamentals, certain evidence-backed options can support overall testosterone optimization.
Evidence-backed options:
- Vitamin D3 (with K2) if blood levels below 40 ng/mL
- Magnesium (glycinate or threonate) – 200-400mg daily
- Zinc – 15-30mg daily if deficient
- Ashwagandha (KSM-66 extract) – 600mg daily
- Tongkat Ali (Longjack) – 200-400mg of quality extract daily
- Boron – 3-10mg daily
Supplements to approach with caution:
- DHEA – Can convert to estrogen in some men
- Tribulus terrestris – Limited evidence for testosterone effects
- Proprietary “testosterone booster” blends with undisclosed amounts
When to Consider Medical Intervention
While lifestyle optimization should always be the foundation, some men may benefit from medical interventions when symptoms persist despite dedicated lifestyle changes.
Signs That Medical Intervention May Be Appropriate
Consider consulting with a hormone specialist if:
- Testosterone levels remain below 350 ng/dL despite lifestyle optimization
- Symptoms significantly impact quality of life
- Testing reveals primary testicular failure
- You have a history of pituitary issues, testicular injury, or other medical factors
Medical Options Beyond TRT
Testosterone replacement therapy (TRT) isn’t the only medical approach. Consider discussing these options with a knowledgeable provider:
- Clomiphene Citrate (Clomid): Works at the brain level to stimulate natural testosterone production; particularly useful for younger men concerned about fertility
- hCG (Human Chorionic Gonadotropin): Mimics luteinizing hormone to stimulate testicular testosterone production while maintaining fertility
- Anastrozole: Reduces excessive conversion of testosterone to estrogen in men with high aromatase activity
- Compounded Creams: Lower-dose testosterone delivered topically for mild cases
Finding the Right Medical Support
Not all healthcare providers are equally knowledgeable about male hormonal health. Consider:
- Seeking specialists in men’s health or functional medicine
- Requesting comprehensive testing beyond basic panels
- Discussing both lifestyle and medical approaches
- Being wary of one-size-fits-all protocols
Monitoring Progress and Adjusting Your Approach
Testosterone optimization is highly individualized. Effective monitoring helps refine your approach:
Tracking Biomarkers
Beyond testosterone itself, these markers help evaluate overall progress:
- Free testosterone and SHBG
- Estradiol (E2)
- Lipid profiles
- Inflammatory markers
- Blood glucose and insulin metrics
- Complete blood count (CBC)
Symptom Journaling
Keep track of:
- Energy patterns throughout the day
- Sleep quality and duration
- Mood and motivation
- Sexual function and libido
- Exercise performance and recovery
- Body composition changes
Adjustment Timeline
Expect a realistic timeline for improvements:
- Sleep and energy changes: Often within 2-3 weeks
- Mood improvements: Typically 3-6 weeks
- Body composition changes: Visible at 6-12 weeks
- Sexual function normalization: Variable, but often 4-12 weeks
- Full optimization: 6 months of consistent implementation
The Personal Responsibility of Hormonal Health
Understanding and optimizing testosterone is ultimately about taking control of your overall health. Low testosterone is rarely an isolated issue but rather a symptom of broader health imbalances that require comprehensive approaches.
By recognizing the early warning signs, implementing evidence-based lifestyle interventions, and seeking appropriate medical support when necessary, men can address the root causes of hormonal decline rather than simply managing symptoms.
The most successful approach combines scientific understanding with personal responsibility—acknowledging that while modern environments pose challenges to hormonal health, we retain significant control over our body’s hormonal expression through daily choices and habits.